Zika History and Current Spread
The Zika virus was first identified in 1947 by scientists who were researching yellow fever in Uganda. They placed a caged rhesus macaque in the Zika forest. After it became sick with a fever, the researchers isolated the virus from its blood. In 1954, in Nigeria, the virus was first isolated from a human. Up until 2007, confirmed human infections were rare and were limited to Africa and Southeast Asia.
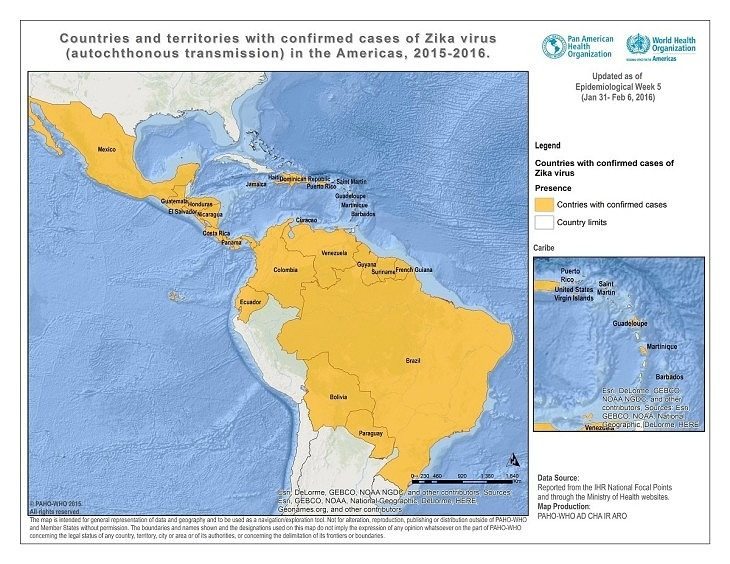
In 2007, an outbreak in Micronesia resulted in 49 confirmed cases and 59 unconfirmed cases. The infections were relatively mild with no associated deaths or hospitalizations. In 2013, the disease reached French Polynesia. In 2014, it reached Brazil and has continued an explosive spread through South America, Central America, and the Caribbean.
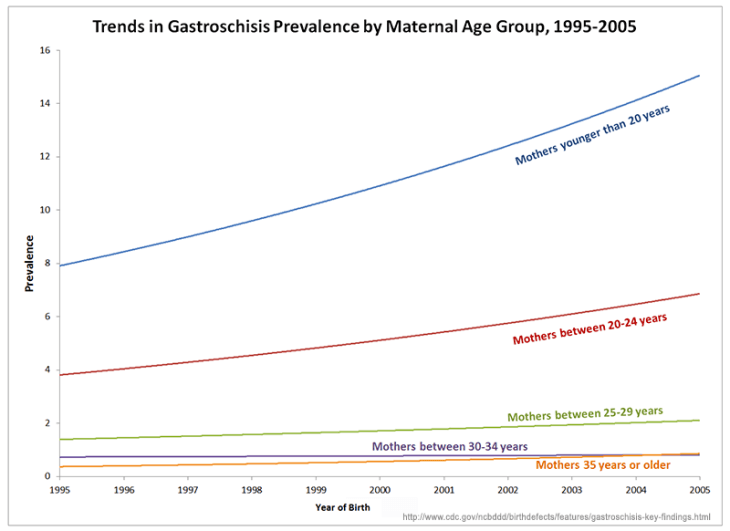
In most cases, the infection is mild. However, a possible, perhaps probable, link between the virus and microcephaly, a severe birth defect whereby an infant is born with an abnormally small head and incomplete brain development, has catapulted this disease from obscurity to the status of a public health emergency and worldwide headline news. Brazilian health authorities have reported more than 3,500 microcephaly cases between October 2015 and January 2016.
…genetically modified mosquitoes are responsible for either the spread of the virus or the rise in birth defects is baseless…
On their website, the World Health Organization states, “Agencies investigating the Zika outbreaks are finding an increasing body of evidence about the link between Zika virus and microcephaly. However, more investigation is needed before we understand the relationship between microcephaly in babies and the Zika virus. Other potential causes are also being investigated.” However, Colombia’s President, Juan Manuel Santos, says there is no evidence that the virus has caused an increase in microcephaly in his country, though they have diagnosed 3,177 pregnant women with the virus.
In January, 2016, The CDC issued a level 2 travel alert to areas where virus transmission is active: Brazil, Colombia, El Salvador, French Guiana, Guatemala, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Suriname, Venezuela, and the U.S. Commonwealth of Puerto Rico. By February, the virus has been found in 20 countries in the Americas.
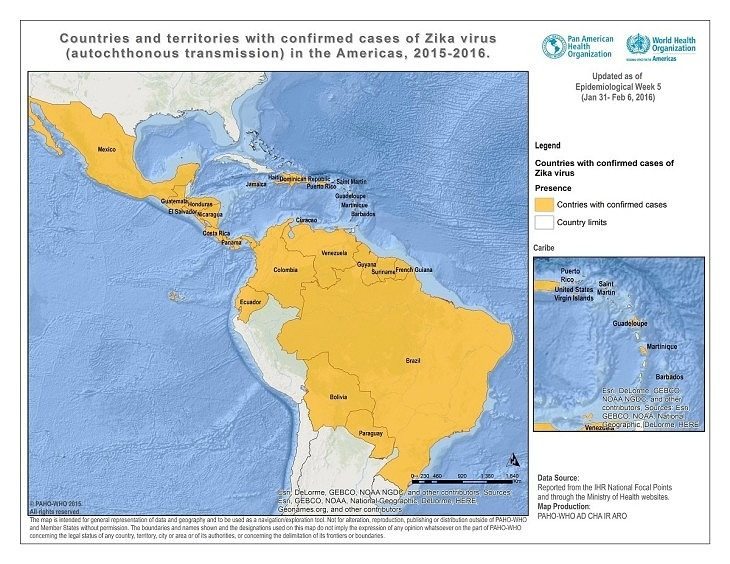
On February 1, 2016, the World Health Organization (WHO) announced that Zika is now considered a public health emergency of international concern. They estimate that the virus will spread throughout the Americas and will infect up to 4 million people by the end of 2016.
How is Zika Spread?
The primary method of transmission is through mosquito bites. There have also been confirmed cases of sexual transmission. The virus is found in saliva, urine, and semen. Semen has been proven to spread the virus. It is not known whether the virus can be transmitted from females to males during unprotected intercourse or through body fluids other than semen.
Some are suggesting the birth defects are due to Brazil’s practice of vaccinating pregnant women with both the DTP and the MMR…
Symptoms of Zika Disease
The Zika virus is typically a mild infection. Up to 80% of those afflicted do not exhibit symptoms. General symptoms are a mild fever, a skin rash, conjunctivitis, headache, muscle and joint pain, and general malaise lasting for 2-7 days. More serious cases can involve neurological and autoimmune complications including Guillain-Barre syndrome, an autoimmune illness in which the immune system attacks the nervous system causing paralysis. (Most people afflicted with Guillain-Barre syndrome recover, though some retain muscle weakness.)
The treatment for most cases is the same as another other mild virus – rest and plenty of fluids.
Spread of Zika Virus to the United States
To date, all of the reported cases of Zika disease in the U.S. are from travelers who contracted the disease outside of the country and brought it home. One man was exposed and infected but had not yet exhibited symptoms before coming home and engaging in unprotected sex with his wife. Both tested positive for Zika when they become ill. A woman in Hawaii gave birth to an infant with a small head after catching the disease while visiting Brazil. There are no known cases of infections due to mosquito bites occurring in the U.S. as of February 7, 2016.
How to Protect Yourself from Catching Zika Disease
The same protocols for eliminating the threat of any mosquito bites apply. First, eliminate breeding grounds. Clean, cover, or get rid of containers that capture standing water. Use screens on windows, keep doors closed, and if you live in an area with a lot of mosquitos, consider sleeping under a mosquito net.
Long sleeves, long pants, and light covered clothing are helpful. You will be told to use insect repellent. Rather than cover your body with insecticide, make your own safe, mosquito/tick repellent.
If your partner has been exposed and you are pregnant or have been trying to become pregnant, use condoms. Scientists do not yet know how long the virus can be contracted after an infection, but this information should be common knowledge soon.
Genetically Modified Mosquitoes and the Zika Virus
Spraying reduces mosquito populations by 30%-50%. The recent release of GM mosquitoes in the CECAP/Eldorado district in Brazil resulted in a 90% reduction in the mosquito population. The release, made before the sudden Zika virus explosion, was targeting mosquitos that carry dengue and chikungunya. These are the same mosquitos that carry Zika. The dengue infection plummeted from 144 cases the previous year to only 1 case after the release of the mosquitos.
The popularity of the belief that genetically modified mosquitoes are responsible for either the spread of the virus or the rise in birth defects is baseless. Male mosquitoes feed on flower nectar; females feed on blood. Only male mosquitoes are genetically modified before being released into the wild. They are equipped with a “kill switch” that successfully kills their offspring before the larvae reach maturity (and can feed on anyone).
It is expected that millions of GM mosquitos will be released to combat the current epidemic.
Conclusion
The Zika virus is a mild virus, one that usually results in no symptoms at all or a low fever and a mild rash. Suddenly this disease is linked with causing a devastating birth defect. This correlation may or may not be causation. Many critics are questioning the probability, especially when comparing Brazil’s outcomes against Colombia’s. Some are suggesting the birth defects are due to Brazil’s practice of vaccinating pregnant women with both the DTP and the MMR vaccines and reminding us that rubella and pertussis components in the DPT vaccine are known to cause microcephaly. Other doctors suggest that a pesticide, Pyriproxyfen (manufactured by Sumitomo Chemical, a Japanese ‘strategic partner’ of Monsanto), which has been added to drinking water tanks to kill mosquito larvae since 2014, may be the source. And of course, some continue to blame the new genetically modified mosquitoes. Although it seems unlikely that genetically modified mosquitoes are a factor, the outcome of these experimental practices remains unknown. What is clear is that something is not adding up. As always, we need to follow the money and see who is benefitting from the situation or who has something to hide. Unfortunately, the list of possible suspects continues to grow.
Further Reading:
Sources: