At first glance, ADHD, chronic fatigue syndrome (CFS), and autism have little in common. When we think of ADHD, we tend to think of hyperactivity, kids zooming from room to room. Chronic fatigue brings up opposite images, of people so wracked with fatigue they can barely get out of bed. Autism suggests children lost in their own world, spinning objects while rocking from side to side. How could they possibly have anything in common?
In order to answer that question, we have to take a serious look at the numbers and understand the diagnostic criteria. If we don’t, the myths and lies will continue to overshadow every effort to understand the real story behind the rise in these debilitating conditions.
ADHD, CFS, and Autism – Epidemics
The first thing these diseases have in common is the fact that all three have reached epidemic proportions. The CDC reports the following statistics:
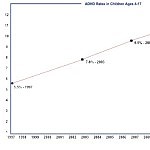
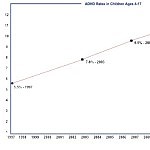
ADHD (> 6 million children in the U.S.)
- 11% of our children have ADHD as of 2011 (up from 7.8% in 2003)
- 1 out of 42 boys
- 1 out of 189 girls
- Rates vary from state to state
Chronic Fatigue Syndrome (up to 2.5 million estimated in the U.S.)
- Between 0.2% and 2.3% of children or adolescents (up to 1.7 million) suffer from CFS.
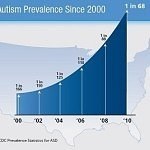
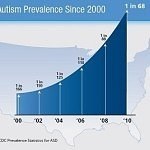
Autism (> 11 million Americans)
- 30% increase from 2012 to 2014
- 5 times more prevalent in boys
- Up 119.4% since 2000, though some current reports now say it has moved from 1 in 68 children to 1 in 50; other reports say 1 in 45.
 Add up the current numbers afflicted with one of these three illnesses, and we are talking about 6% of the population – without counting adults with ADHD.
Add up the current numbers afflicted with one of these three illnesses, and we are talking about 6% of the population – without counting adults with ADHD.
Public Perception of ADHD, CFS, and Autism
The perception of these three illnesses are skewed and no clarity is in sight.
ADHD Myths and Propaganda
- ADHD is horribly over diagnosed
- Children can’t sit still in a classroom; ergo, hyperactivity is normal
- All active little boys are diagnosed with ADHD
- The rising numbers of ADHD cases are all due to over diagnosis
- Kids diagnosed with ADHD are spoiled children who don’t behave
For decades, we have heard the number of children with ADHD is dramatically over reported. This myth has resulted in the public ignoring the alarming rise in the number of children (and children who have grown into adulthood) afflicted by this disorder.
The idea that children are diagnosed with ADHD just to medicate them is ludicrous. That might be a good argument if tranquilizers were the medication prescribed for ADHD, but the opposite is true. Put any child without ADHD on amphetamines and the child will become hyper, anxious, and out of control. Amphetamines have the opposite effect on most of the children with ADHD. The child is able to calm down, focus, concentrate and control impulsivity. (Note: We are NOT advocating the use of medication to treat ADHD).
As long as we continue to discount the validity of this diagnosis, the sheer number of afflicted children won’t alarm us, and we won’t shake the boat by looking for the cause or causes.
Chronic Fatigue Myths and Propaganda
- It’s all in their head
- They’re not sick, they’re lazy
- There is no such thing as chronic fatigue syndrome
Like ADHD, chronic fatigue syndrome has been discounted, but in this case, it is dismissed as a non-disease. It was even given a derogatory nickname, the yuppie flu. Severe chronic fatigue is a devastating illness, and yet, due to propaganda within the medical field and vague diagnostics, many doctors believe it to be psychosomatic. Patients are dismissed as attention seekers, histrionics, and malingerers. This is an all too common occurrence whenever doctors cannot find a cause or determine a diagnosis for autoimmune or neurological symptoms unless evidence can clearly be shown through a blood test, an MRI, or some other definitive test.
Although it is estimated that twice as many Americans suffer from chronic fatigue syndrome as HIV, the National Institutes of Health budgeted a paltry $6 million in funding for chronic fatigue research for 2016 while HIV/AIDS research is budgeted at $3.1 billion. (Compare this amount to headaches budgeted at $25 million – migraines have a separate budget of $21 million.) So we have a serious, debilitating illness on the rise that affects a huge number of Americans, but since it became an issue, it has been discounted and largely ignored.
Autism Myths and Propaganda
- The change in diagnostic criteria is responsible for the increase in rates.
- Vaccines have no association with autism.
- Autism is an entirely genetic disease.
Autism was a rare diagnosis in the last century. In the 1980s, estimates from multiple studies suggest autism affected 1 in 10,000 children. In a mere 20 years, the year 2000, that number rose to 1 in 150 children. By 2010, the number was 1 in 68. The 2010 numbers are still being reported as the official numbers by the CDC and used by other organizations, though some are now estimating 1 in 45 children. Dr. Stephanie Seneff, Senior Research Scientist from MIT, stated, “At today’s rate, by 2025, one in two children will be autistic.”
While there is truth to the claim that new diagnostic parameters created a bump in the numbers, the increase happened once. Once! And again the numbers climbed and continue to climb. Like ADHD and CFS, autism is a relatively new disease with the first case diagnosed and named in 1938.
The autism epidemic is huge. How can we continue to deny the truth? The numbers are frightening and not just for the afflicted child and parents. The impact on our society will be tremendous when the children with severe autism grow to adulthood. Who will care for them when their parents are no longer able to provide for them?
Diagnostic Criteria
The myth that “ADHD is horribly over diagnosed,” is a bit harder to swallow when you understand the diagnostic criteria, when you appreciate the severity of the impact ADHD has on a child and his/her family, and when you see how unlikely it is for a child to be improperly diagnosed.
CDC Diagnostic Criteria for Attention Deficit Hyperactivity Disorder (ADHD)
The CDC uses the DSM V (Diagnostic and Statistical Manual V – the diagnostic manual for mental health professionals) definition as follows:
“People with ADHD show a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development.”
Inattention: Six or more symptoms of inattention for children up to age 16, or five or more for adolescents 17 and older and adults; symptoms of inattention have been present for at least 6 months, and they are inappropriate for developmental level:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Often has trouble holding attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., loses focus, side-tracked).
- Often has trouble organizing tasks and activities.
- Often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of time (such as schoolwork or homework).
- Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted.
- Is often forgetful in daily activities.
Hyperactivity and Impulsivity: Six or more symptoms of hyperactivity-impulsivity for children up to age 16, or five or more for adolescents 17 and older and adults; symptoms of hyperactivity-impulsivity have been present for at least 6 months to an extent that is disruptive and inappropriate for the person’s developmental level:
- Often fidgets with or taps hands or feet, or squirms in seat.
- Often leaves seat in situations when remaining seated is expected.
- Often runs about or climbs in situations where it is not appropriate (adolescents or adults may be limited to feeling restless).
- Often unable to play or take part in leisure activities quietly.
- Is often “on the go” acting as if “driven by a motor”.
- Often talks excessively.
- Often blurts out an answer before a question has been completed.
- Often has trouble waiting his/her turn.
- Often interrupts or intrudes on others (e.g., butts into conversations or games).
In addition, the following conditions must be met
- Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
- Several symptoms are present in two or more setting, (e.g., at home, school or work; with friends or relatives; in other activities).
- There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
- The symptoms do not happen only during the course of schizophrenia or another psychotic disorder. The symptoms are not better explained by another mental disorder (e.g. Mood Disorder, Anxiety Disorder, Dissociative Disorder, or a Personality Disorder).”
DSM-V Diagnostic Criteria for Autism Spectrum Disorder
Diagnostic Criteria
Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive, see text):
- Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions.
- Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication.
- Deficits in developing, maintaining, and understanding relationships, ranging, for example, from difficulties adjusting behavior to suit various social contexts; to difficulties in sharing imaginative play or in making friends; to absence of interest in peers.
Specify current severity
Severity is based on social communication impairments and restricted repetitive patterns of behavior (see Table 2)
Restricted, repetitive patterns of behavior, interests, or activities, as manifested by at least two of the following, currently or by history (examples are illustrative, not exhaustive; see text):
- Stereotyped or repetitive motor movements, use of objects, or speech (e.g., simple motor stereotypies, lining up toys or flipping objects, echolalia, idiosyncratic phrases).
- Insistence on sameness, inflexible adherence to routines, or ritualized patterns or verbal nonverbal behavior (e.g., extreme distress at small changes, difficulties with transitions, rigid thinking patterns, greeting rituals, need to take same route or eat food every day).
- Highly restricted, fixated interests that are abnormal in intensity or focus (e.g, strong attachment to or preoccupation with unusual objects, excessively circumscribed or perseverative interest).
- Hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment (e.g., apparent indifference to pain/temperature, adverse response to specific sounds or textures, excessive smelling or touching of objects, visual fascination with lights or movement).
Specify current severity
Severity is based on social communication impairments and restricted, repetitive patterns of behavior (see Table 2)
- Symptoms must be present in the early developmental period (but may not become fully manifest until social demands exceed limited capacities, or may be masked by learned strategies in later life).
- Symptoms cause clinically significant impairment in social, occupational, or other important areas of current functioning.
- These disturbances are not better explained by intellectual disability (intellectual developmental disorder) or global developmental delay. Intellectual disability and autism spectrum disorder frequently co-occur; to make comorbid diagnoses of autism spectrum disorder and intellectual disability, social communication should be below that expected for general developmental level.
Note: Individuals with a well-established DSM-IV diagnosis of autistic disorder, Asperger’s disorder, or pervasive developmental disorder not otherwise specified should be given the diagnosis of autism spectrum disorder. Individuals who have marked deficits in social communication, but whose symptoms do not otherwise meet criteria for autism spectrum disorder, should be evaluated for social (pragmatic) communication disorder.
Specify if:
- With or without accompanying intellectual impairment
- With or without accompanying language impairment
- Associated with a known medical or genetic condition or environmental factor
(Coding note: Use additional code to identify the associated medical or genetic condition.)
- Associated with another neurodevelopmental, mental, or behavioral disorder
(Coding note: Use additional code[s] to identify the associated neurodevelopmental, mental, or behavioral disorder[s].)
- With catatonia (refer to the criteria for catatonia associated with another mental disorder, pp. 119-120, for definition) (Coding note: Use additional code 293.89 [F06.1] catatonia associated with autism spectrum disorder to indicate the presence of the comorbid catatonia.)
Table 2 Severity levels for autism spectrum disorder
| Severity level |
Social communication |
Restricted, repetitive behaviors |
Level 3
“Requiring very substantial support” |
Severe deficits in verbal and nonverbal social communication skills cause severe impairments in functioning, very limited initiation of social interactions, and minimal response to social overtures from others. For example, a person with few words of intelligible speech who rarely initiates interaction and, when he or she does, makes unusual approaches to meet needs only and responds to only very direct social approaches |
Inflexibility of behavior, extreme difficulty coping with change, or other restricted/repetitive behaviors markedly interfere with functioning in all spheres. Great distress/difficulty changing focus or action. |
Level 2
“Requiring substantial support” |
Marked deficits in verbal and nonverbal social communication skills; social impairments apparent even with supports in place; limited initiation of social interactions; and reduced or abnormal responses to social overtures from others. For example, a person who speaks simple sentences, whose interaction is limited to narrow special interests, and how has markedly odd nonverbal communication. |
Inflexibility of behavior, difficulty coping with change, or other restricted/repetitive behaviors appear frequently enough to be obvious to the casual observer and interfere with functioning in a variety of contexts. Distress and/or difficulty changing focus or action. |
Level 1
“Requiring support” |
Without supports in place, deficits in social communication cause noticeable impairments. Difficulty initiating social interactions, and clear examples of atypical or unsuccessful response to social overtures of others. May appear to have decreased interest in social interactions. For example, a person who is able to speak in full sentences and engages in communication but who to- and-fro conversation with others fails, and whose attempts to make friends are odd and typically unsuccessful. |
Inflexibility of behavior causes significant interference with functioning in one or more contexts. Difficulty switching between activities. Problems of organization and planning hamper independence. |
CDC Diagnosis of Chronic Fatigue Syndrome
A clinician should consider a diagnosis of CFS if these three criteria are met:
- The individual has unexplained, persistent fatigue for 6 months or longer that is not due to ongoing exertion, is not substantially relieved by rest, has begun recently (is not lifelong)
- The fatigue significantly interferes with daily activities and work
- The individual has had 4 or more of the following 8 symptoms:
- post-exertion malaise lasting more than 24 hours
- unrefreshing sleep
- significant impairment of short-term memory or concentration
- muscle pain
- pain in the joints without swelling or redness
- a sore throat that is frequent or recurring
- tender lymph nodes in the neck or armpit
- headaches of a new type, pattern, or severity
Association Not Cause
In a recent interview, Judy Mikovits, PhD eloquently explained the scientific definition of cause and effect versus association. In order to say that a disease is “caused” by something, there has to be a clear cause and effect that is the same each time. For instance, mumps is caused by a particular virus – every time. It isn’t caused by a virus in one case and a bacteria in another.
Most of us are used to defining an illness through cause and effect of a bacterial or viral infection. Contagious illness and trauma are well understood by the general public. Autoimmune diseases and neurological diseases are much harder to understand, and this is true for medical professionals as well as the general public.
There are few definitive diagnostic tests for ADHD, CFS, or autism. Most of the diagnostic criteria is based on observation and patient report.
However, MRI studies with children diagnosed with ADHD have shown lower activity in the frontal lobes as well as recent discoveries of disrupted connections between different areas of the brain showing structural and functional abnormalities.
In 2011, Judy Mikovitz, PhD, found an association between gammaretrovirus XMRV and chronic fatigue syndrome and autism. Retroviruses damage DNA and cause autoimmune and neurological damage. Judy believes up to one-third of our vaccines are contaminated with this retrovirus that accidently contaminated cell lines in the labs where vaccines were made.
Fragile X syndrome is “…the most common inherited cause of intellectual disabilities. It is also the most common known cause of autism.” – Fraxa Research Foundation website.
Fragile X is caused by a defect in the FMR1 gene. The gene shuts down and fails to produce a protein vital for brain development. Symptoms include mild to severe attention deficit and hyperactivity and autism. One can’t help but wonder if damage to the FMR1 gene is caused by a retrovirus.
What Do We Know?
Vaccines are certainly proving to be a major factor associated with ADHD, autism, autoimmune disease, and other diseases with mercury poisoning, retrovirus exposure, and damage from aluminum and other toxins all playing a part. But vaccines are not the only toxins we are exposed to and clearly not the only factor in play. We know that there are multiple means to damage the immune system and the neurological system and that damage is cumulative.
Damage begins in utero. A fetus pulls mercury out of its mother’s body. It is tragic that doctors continue to recommend pregnant women get vaccines, especially the flu shot that contains mercury.
In addition to vaccines, environmental toxins contribute to damage. Herbicides and pesticides accumulate in our tissues along with the countless chemicals we are exposed to every day.
Conclusion
If we are to stop the current epidemic of neurological and autoimmune diseases including ADHD, CFS, and autism, we have to stop poisoning our bodies and our children’s bodies with chemicals and heavy metals. We need to clean up our food, eliminate toxin exposure in our homes and workplaces, and stop poisoning ourselves and our children through vaccines. The numbers don’t lie. ADHD, CFS, and autism are the result of our polluted lives and a vaccine schedule that would defy common sense even if our vaccines were safe and effective. Too many of us are sick. Too many children are sick. It’s time we stand up and demand change.
Further Reading:
Sources: